What is excessive sweating (Primary Focal Hyperhidrosis)?
Primary focal hyperhidrosis is excessive sweating localized to the palms, soles of the feet, head, face, and armpits without any underlying conditions such as neurological diseases or drugs that prompt excessive sweating.
If the excessive sweating is localized to the palms or soles of the feet, the condition is referred to as ‘primary palmoplantar hyperhidrosis.’ In the same way, if the sweating is prominent only on the head and face, then the term ‘primary craniofacial hyperhidrosis’ applies. Whereas if the sweating is prominent only on the armpits, the condition is referred to as ‘primary axillary hyperhidrosis.’
Therefore primary focal hyperhidrosis is excessive sweating localized on the palms, soles of the feet, head, face, or armpits, or it can also occur on several of these areas simultaneously.
Although there is no clearly known cause to primary focal hyperhidrosis, the condition is thought to be a result of hyperactivity of sweat glands in the area.
By contrast, focal hyperhidrosis that has obvious causes, such as neurological diseases or certain drug administrations, is referred to as ‘secondary hyperhidrosis’.
When excessive sweating is not localized on the palms, soles of the feet, head, face, or armpits, then the condition is referred to as ‘generalized hyperhidrosis’.
It is estimated that the prevalence of primary focal hyperhidrosis is about 5% of the population worldwide (it depends on the statistics) and less than 50% of the hyperhidrotic patients seek medical attention.
If the excessive sweating is localized to the palms or soles of the feet, the condition is referred to as ‘primary palmoplantar hyperhidrosis.’ In the same way, if the sweating is prominent only on the head and face, then the term ‘primary craniofacial hyperhidrosis’ applies. Whereas if the sweating is prominent only on the armpits, the condition is referred to as ‘primary axillary hyperhidrosis.’
Therefore primary focal hyperhidrosis is excessive sweating localized on the palms, soles of the feet, head, face, or armpits, or it can also occur on several of these areas simultaneously.
Although there is no clearly known cause to primary focal hyperhidrosis, the condition is thought to be a result of hyperactivity of sweat glands in the area.
By contrast, focal hyperhidrosis that has obvious causes, such as neurological diseases or certain drug administrations, is referred to as ‘secondary hyperhidrosis’.
When excessive sweating is not localized on the palms, soles of the feet, head, face, or armpits, then the condition is referred to as ‘generalized hyperhidrosis’.
It is estimated that the prevalence of primary focal hyperhidrosis is about 5% of the population worldwide (it depends on the statistics) and less than 50% of the hyperhidrotic patients seek medical attention.

|

|

|
Normal sweating and excessive sweating (Hyperhidrosis)
People sweat in a hot summer day or because of exercise. This occurs in order to cool the body, i.e. to prevent it from overheating. This type of sweating is caused by thermal stimuli (thermal sweating) and is a normal physiological response. People may sweat when they feel anxious, stressed, or excited (emotional/psychological sweating), or when they eat hot/spicy food (gustatory sweating).
Sweat comes out from sweat glands called ‘eccrine sweat glands.’ Sweating occurs once the receptors receive a substance called ‘acetylcholine,’ which is released from nearby sympathetic nerves after the brain perceives thermal or psychological stimuli (Figure 1).
The affected area is influenced by the type of stimuli that provoke sweating. Psychological stimuli appear to mainly provoke sweating on the palms and soles of the feet. This sweat is caused by emotional stress such as fear, anxiety or excitement as seen when you have ‘sweaty hands.’ On the other hand, both thermal and psychological stimuli can cause sweating in the armpits. For example, one could break into a cold sweat without thermal stimuli indicating that a cold sweat is caused by psychological stimuli. Gustatory stimuli, in addition to thermal and psychological stimuli can cause sweating on the head and face.
In primary focal hyperhidrosis, these sweating processes occur at the level where they may interfere with one’s daily activity (Figure 2).
Sweat comes out from sweat glands called ‘eccrine sweat glands.’ Sweating occurs once the receptors receive a substance called ‘acetylcholine,’ which is released from nearby sympathetic nerves after the brain perceives thermal or psychological stimuli (Figure 1).
The affected area is influenced by the type of stimuli that provoke sweating. Psychological stimuli appear to mainly provoke sweating on the palms and soles of the feet. This sweat is caused by emotional stress such as fear, anxiety or excitement as seen when you have ‘sweaty hands.’ On the other hand, both thermal and psychological stimuli can cause sweating in the armpits. For example, one could break into a cold sweat without thermal stimuli indicating that a cold sweat is caused by psychological stimuli. Gustatory stimuli, in addition to thermal and psychological stimuli can cause sweating on the head and face.
In primary focal hyperhidrosis, these sweating processes occur at the level where they may interfere with one’s daily activity (Figure 2).
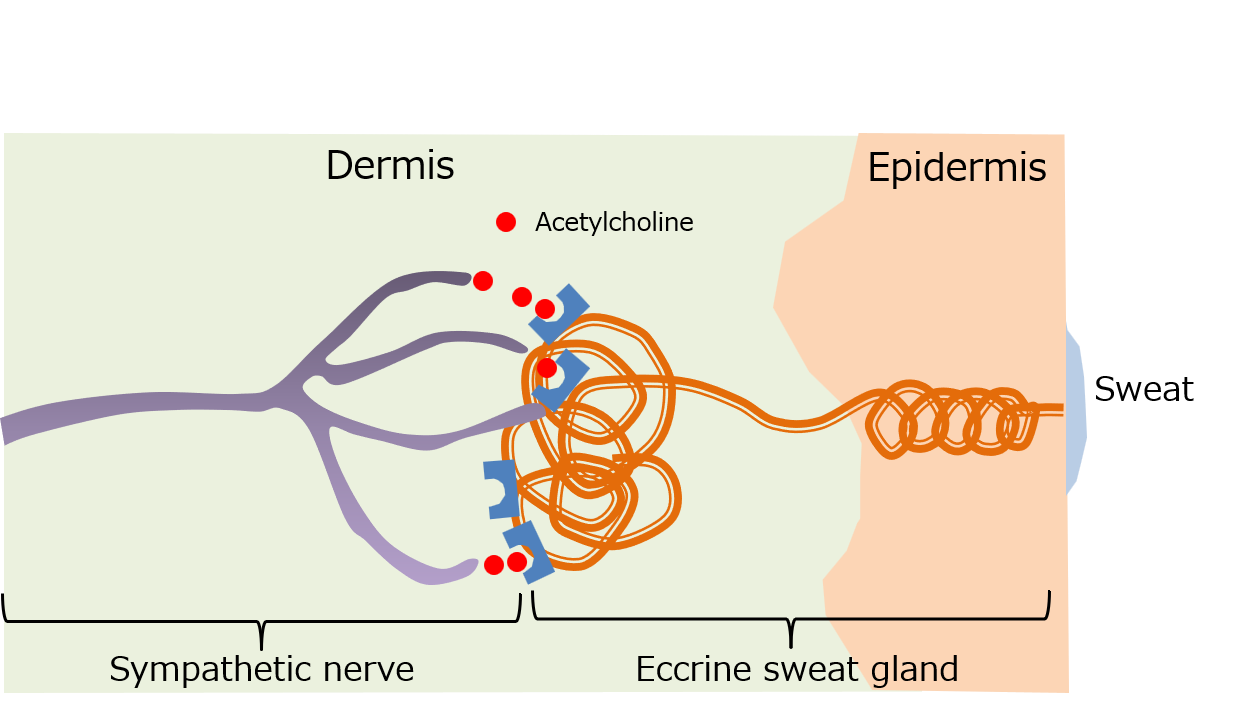
Figure 1. Mechanism of sweating
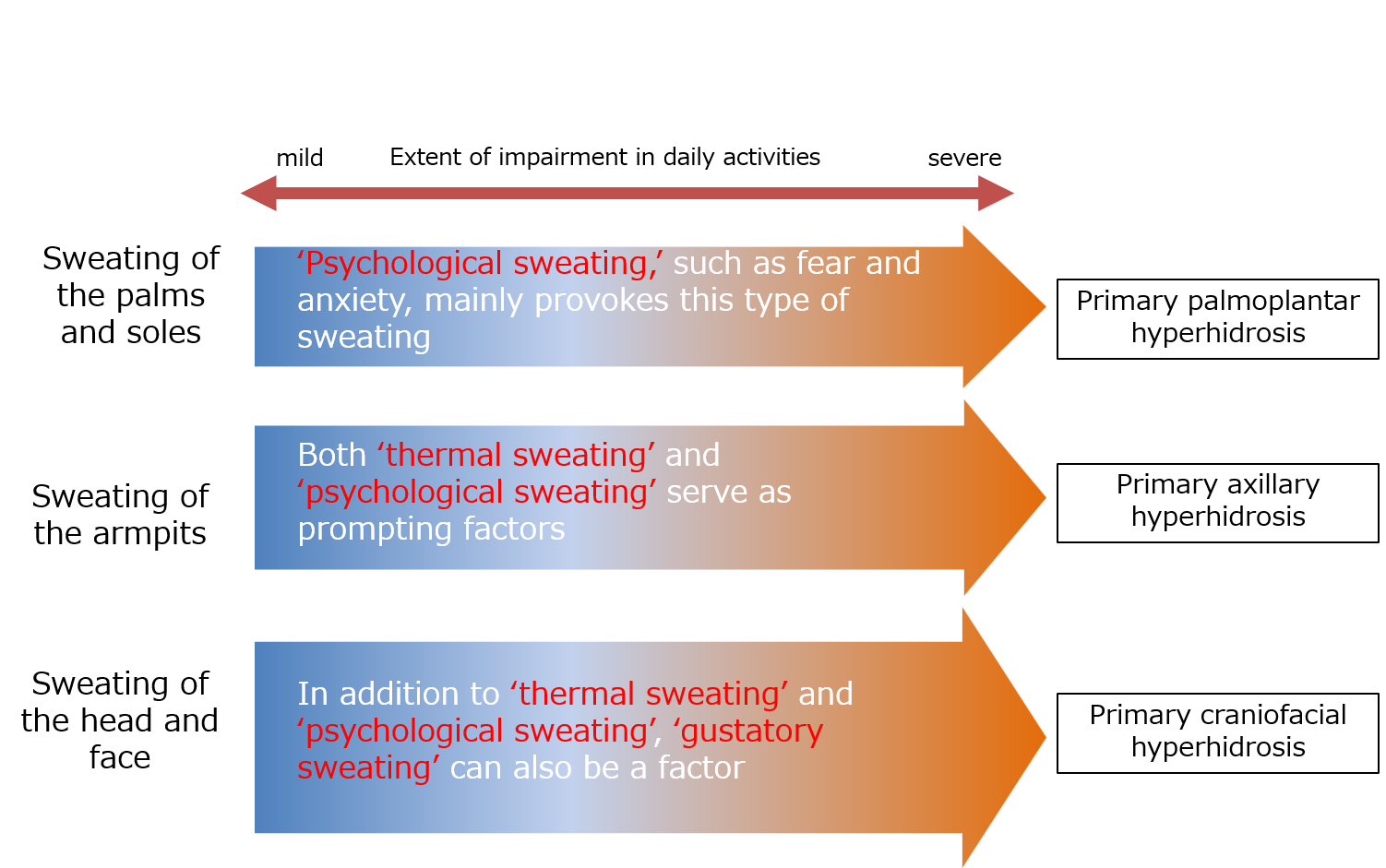
Figure 2. Normal sweating and excessive sweating (hyperhidrosis)
The diagnosis of primary focal hyperhidrosis
Several diagnostic approaches or criteria have been reported to date. The following is an example of the aforementioned criteria.
A diagnosis can occur if excessive sweating continues for six months or longer, along with four or more of the following seven items*:
1. Sweating occurs in the axillary (under the armpits), soles of the feet, palms, face, or head
2. Sweating is not isolated to one side of the body
3. Sweating is absent at night
4. Sweating occurs at least once a week
5. Sweating begins at 25 years of age or younger
6. There is a family history of hyperhidrosis
7. Symptoms cause impairment in daily activities
Some examples of an impairment in daily activities, according to our patients diagnosed with hyperhidrosis, are the following:
・pieces of paper given at school get blotchy with sweat
・pencils become slippery due to sweat
・noticeable sweating on the head occurs when others are not sweating
A diagnosis can occur if excessive sweating continues for six months or longer, along with four or more of the following seven items*:
1. Sweating occurs in the axillary (under the armpits), soles of the feet, palms, face, or head
2. Sweating is not isolated to one side of the body
3. Sweating is absent at night
4. Sweating occurs at least once a week
5. Sweating begins at 25 years of age or younger
6. There is a family history of hyperhidrosis
7. Symptoms cause impairment in daily activities
Some examples of an impairment in daily activities, according to our patients diagnosed with hyperhidrosis, are the following:
・pieces of paper given at school get blotchy with sweat
・pencils become slippery due to sweat
・noticeable sweating on the head occurs when others are not sweating
*J Am Acad Dermatol. 2011; 64: 690-5
Assessment of the extent of sweating at our clinic
As an assessment method of the extent of sweating, various methods have been reported. We, at the clinic, use a special sheet that turns black as it gets into contact with water. Photo 1 was taken 1 minute after a patient with severe primary palmoplantar hyperhidrosis placed his palms on the sheet. In the case of primary palmoplantar hyperhidrosis, the degree of sweating varies depending on the timing of the measurement and other factors, but we believe it is useful as a reference.

Photo 1. Well demarcated figure of the palms are obvious on a special sheet that turned black after 1-minute placement of the hands of a patient with severe palmoplantar hyperhidrosis.
Severity of primary focal hyperhidrosis
An index of the severity of primary focal hyperhidrosis, HDSS (Hyperhidrosis disease severity scale) is the frequently used index that divides levels of severity of sweating into four degrees according to the degree to which sweating interferes with daily activities. Item 3, and 4 are considered as severe.
How would you rate the severity of your hyperhidrosis?
1. My sweating is never noticeable and never interferes with my daily activities.
2. My sweating is tolerable but sometimes interferes with my daily activities.
3. My sweating is barely tolerable and frequently interferes with my daily activities.
4. My sweating is intolerable and always interferes with my daily activities.
How would you rate the severity of your hyperhidrosis?
1. My sweating is never noticeable and never interferes with my daily activities.
2. My sweating is tolerable but sometimes interferes with my daily activities.
3. My sweating is barely tolerable and frequently interferes with my daily activities.
4. My sweating is intolerable and always interferes with my daily activities.
J Am Acad Dermatol. 2004; 51: 241-248
Treatment of focal hyperhidrosis
In addition to the conventional treatment of primary focal hyperhidrosis with topical aluminum chloride (thought to be effective by occluding eccrine sweat glands: not covered by national health insurance), topical anticholinergic agents such as Ecclock gel® and Rapifort Wipes® for axillary hyperhidrosis are now covered by insurance, which broadened the therapeutic options.
We also offer treatment with ‘tap water iontophoresis’ at the clinic for patients with palmoplantar hyperhidrosis (palms and soles), which is covered by national health insurance.
We also offer treatment with ‘tap water iontophoresis’ at the clinic for patients with palmoplantar hyperhidrosis (palms and soles), which is covered by national health insurance.
Treatment of palmoplantar hyperhidrosis with tap-water iontophoresis
Tap water iontophoresis is applied by immersing hands or soles of the feet in trays filled with tap water and applying electric current (Photo 2). Tap water iontophoresis has been reported for more than 40 years in various scientific reports to suppress the sweating in palmoplantar hyperhidrosis.
It is speculated that the hydrogen ions generated when electric current is applied to tap water occlude the sweat pores and inhibit sweating.
We, at the clinic, use a device called Iontophoresis IP-30PLUS (Photo 3).
Tap water iontophoresis is covered by insurance. The fee for one treatment is 660 yen for a patient who pays 30% of the total cost, if the treatment is performed only on the palms/sole of the feet (consultation fee will be charged separately).
The treatment begins with 5 to 10 minutes duration of electric current application once or twice a week, and then the extent of the currency and duration will be adjusted. After 4-5 sessions, the treatment interval will be increased as certain effect is obtained.
It is speculated that the hydrogen ions generated when electric current is applied to tap water occlude the sweat pores and inhibit sweating.
We, at the clinic, use a device called Iontophoresis IP-30PLUS (Photo 3).
Tap water iontophoresis is covered by insurance. The fee for one treatment is 660 yen for a patient who pays 30% of the total cost, if the treatment is performed only on the palms/sole of the feet (consultation fee will be charged separately).
The treatment begins with 5 to 10 minutes duration of electric current application once or twice a week, and then the extent of the currency and duration will be adjusted. After 4-5 sessions, the treatment interval will be increased as certain effect is obtained.

Photo 2. Treatment with tap-water iontophoresis
Photo 3. Iontophoresis IP-30 PLUS
Topical anticholinergics for excessive sweating of the armpits (primary axillary hyperhidrosis)
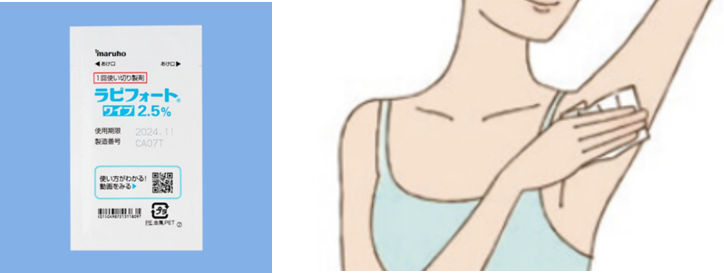
At present, two types of topical-type anticholinergics are used for underarm excessive sweating (primary axillary hyperhidrosis): ECCLOCK gel (Sofpironium bromide), and Rapifort Wipes (Glycopyrronium tosylate).
They both are covered by the national health insurance. They achieve their therapeutic effect by blocking the acetylcholine receptor called ‘M3’, rendering the sympathetic nervous stimuli brought by acetylcholine ineffective.
ECCLOCK gel 5% is applicable to the patients of primary axillary hyperhidrosis of 12 years and older. The container is so designed that one can apply the gel on the armpits without touching the gel, which helps avoid the unwanted side effects of the inhibition of the action of acetylcholine elsewhere (e.g. rubbing the eyes with gel-covered hands may cause the pupils to dilate, which might make the patient feel dazzled)
Rapifort wipes 2.5% is applicable to the patient 9 years and older. It is a sheet-type medication applied directly by wiping the armpit with the medicated sheet (Qbrexza® 3.75% is its equivalent medication in the US). After application of the wipes, one needs to wash the hands well.
They both are covered by the national health insurance. They achieve their therapeutic effect by blocking the acetylcholine receptor called ‘M3’, rendering the sympathetic nervous stimuli brought by acetylcholine ineffective.
ECCLOCK gel 5% is applicable to the patients of primary axillary hyperhidrosis of 12 years and older. The container is so designed that one can apply the gel on the armpits without touching the gel, which helps avoid the unwanted side effects of the inhibition of the action of acetylcholine elsewhere (e.g. rubbing the eyes with gel-covered hands may cause the pupils to dilate, which might make the patient feel dazzled)
Rapifort wipes 2.5% is applicable to the patient 9 years and older. It is a sheet-type medication applied directly by wiping the armpit with the medicated sheet (Qbrexza® 3.75% is its equivalent medication in the US). After application of the wipes, one needs to wash the hands well.

Rapifort wipes 2.5% is applicable to the patient 9 years and older. It is a sheet-type medication applied directly by wiping the armpit with the medicated sheet (Qbrexza® 3.75% is its equivalent medication in the US). After application of the wipes, one needs to wash the hands well.
Topical aluminum chloride application for hyperhidrosis
Aluminum chloride is widely used as a topical treatment for hyperhidrosis (applied directly to the armpits, palms, and soles of the feet). Since there is NO topical aluminum chloride covered by national health insurance at present, it is usually prescribed as an in-hospital preparation.
The solution is thought to exert its effect through the obstruction of the sweat duct.
Side effects include irritant dermatitis (irritation at the site of topical application due to the components of the topical aluminum chloride).
At the clinic, we deal with a spray-type aluminum chloride for 750 yen, which does not contain alcohol, one of the known irritants (Photo 4).
The solution is thought to exert its effect through the obstruction of the sweat duct.
Side effects include irritant dermatitis (irritation at the site of topical application due to the components of the topical aluminum chloride).
At the clinic, we deal with a spray-type aluminum chloride for 750 yen, which does not contain alcohol, one of the known irritants (Photo 4).
Photo 4. Aluminum chloride solution